Mandible ( Jaw) Reconstruction
- Home
- Mandible ( Jaw) Reconstruction
About Mandible ( Jaw) Reconstruction
Mandible reconstruction is a surgery to rebuild the lower jaw (mandible) when it’s been removed due to cancer, trauma, or infection. The goal is to restore the function, shape, and appearance of the jaw—so the person can chew, speak, and look normal again
The options available for Mandible reconstruction are:
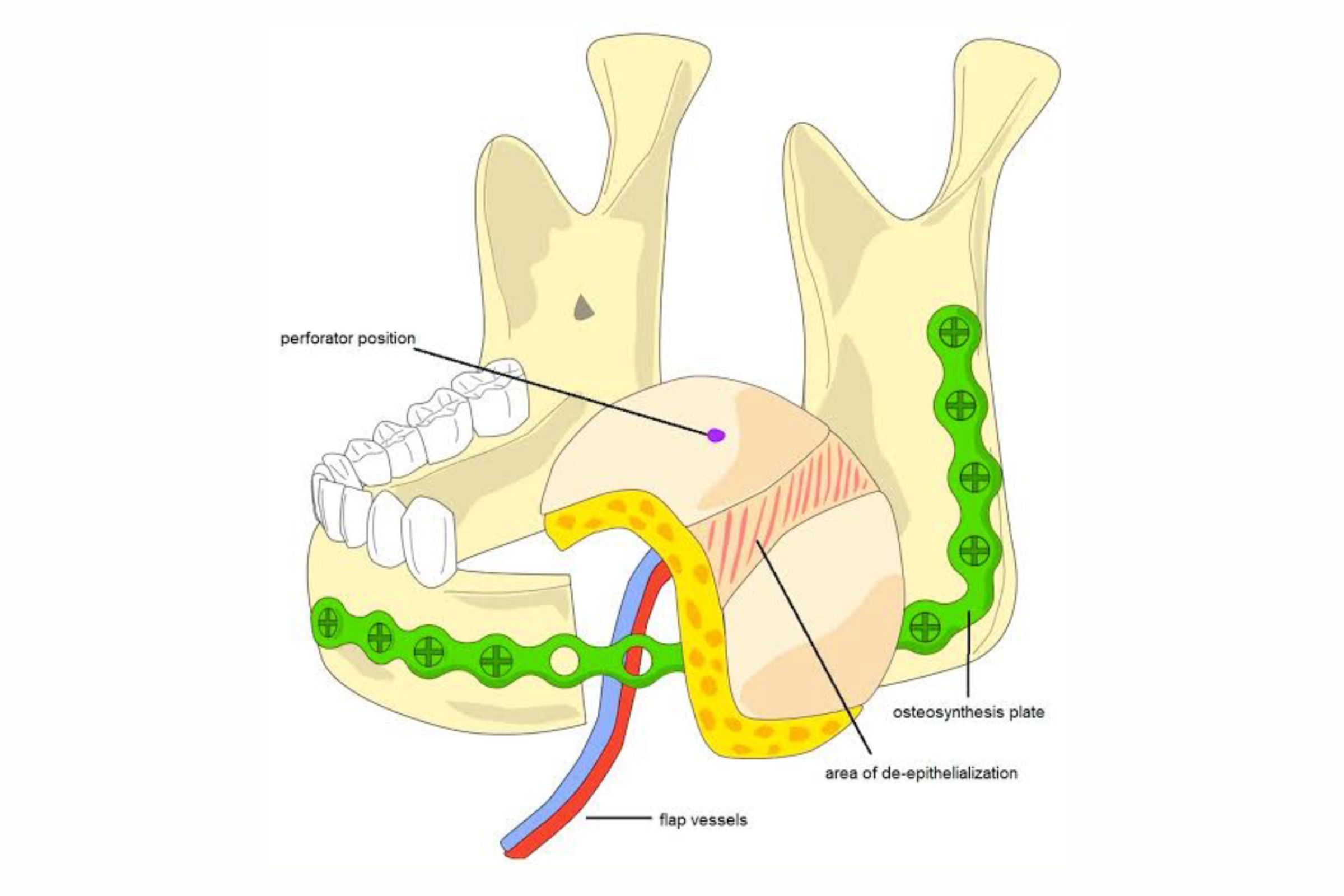
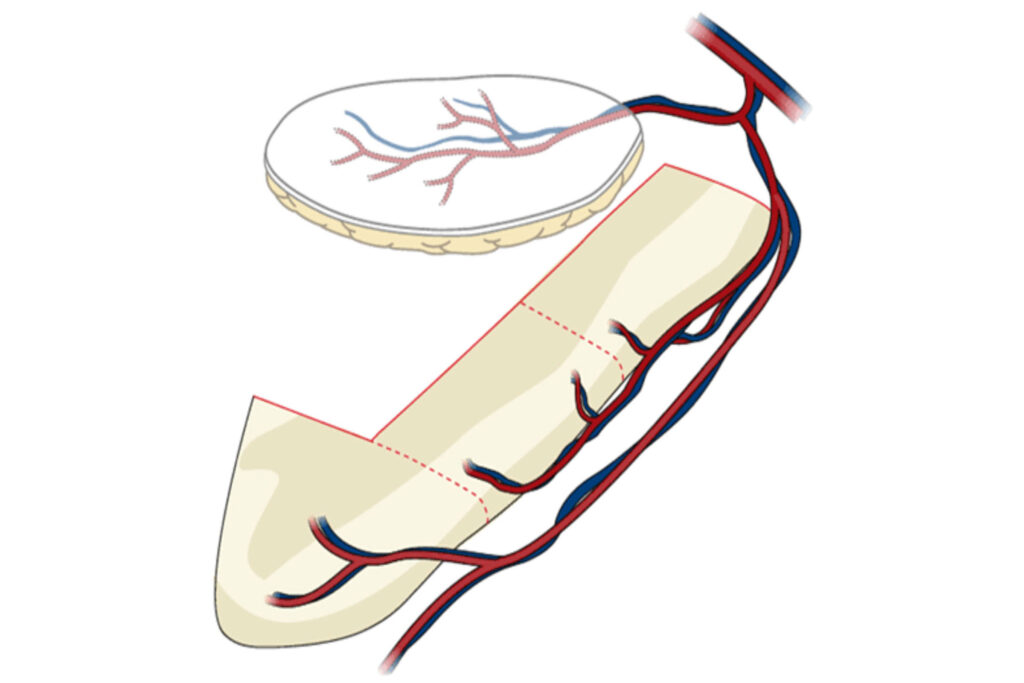
Free Fibula Osteocutaenous Flap FFOCF:
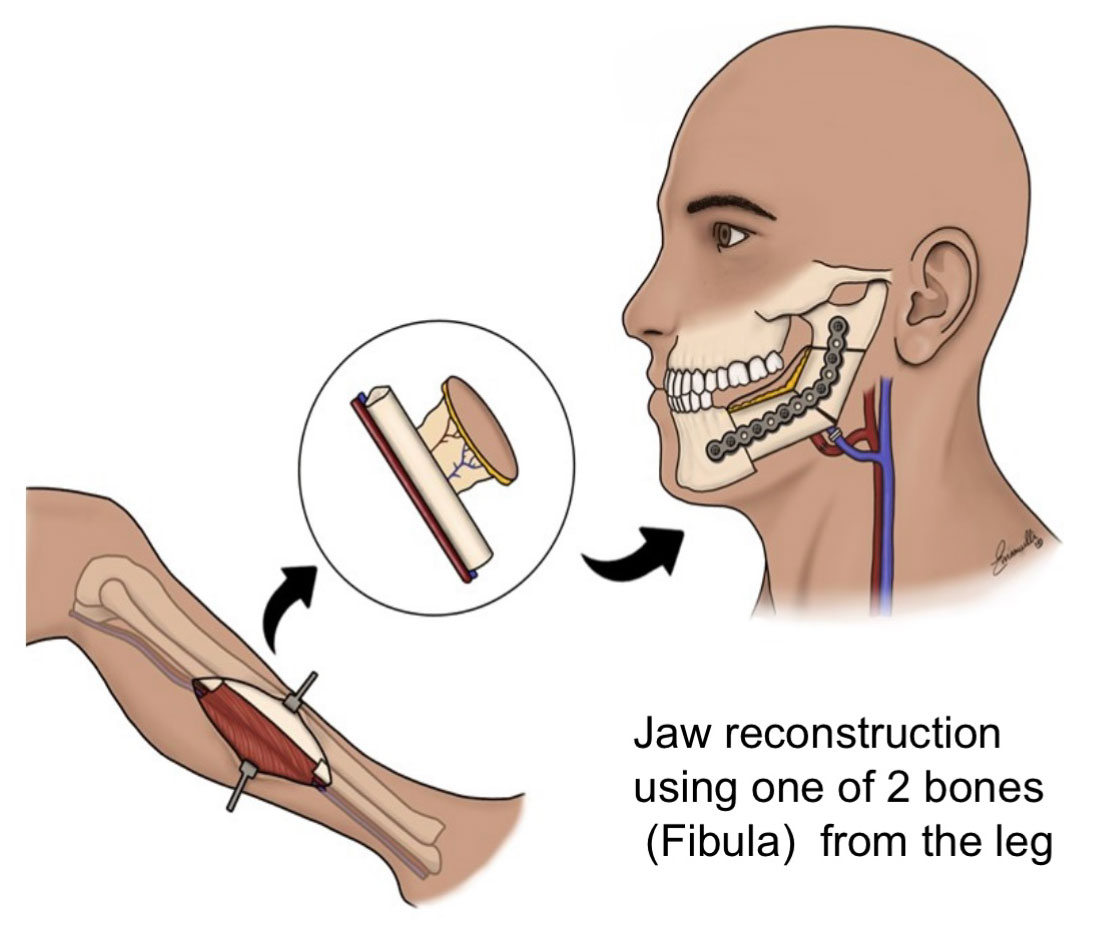
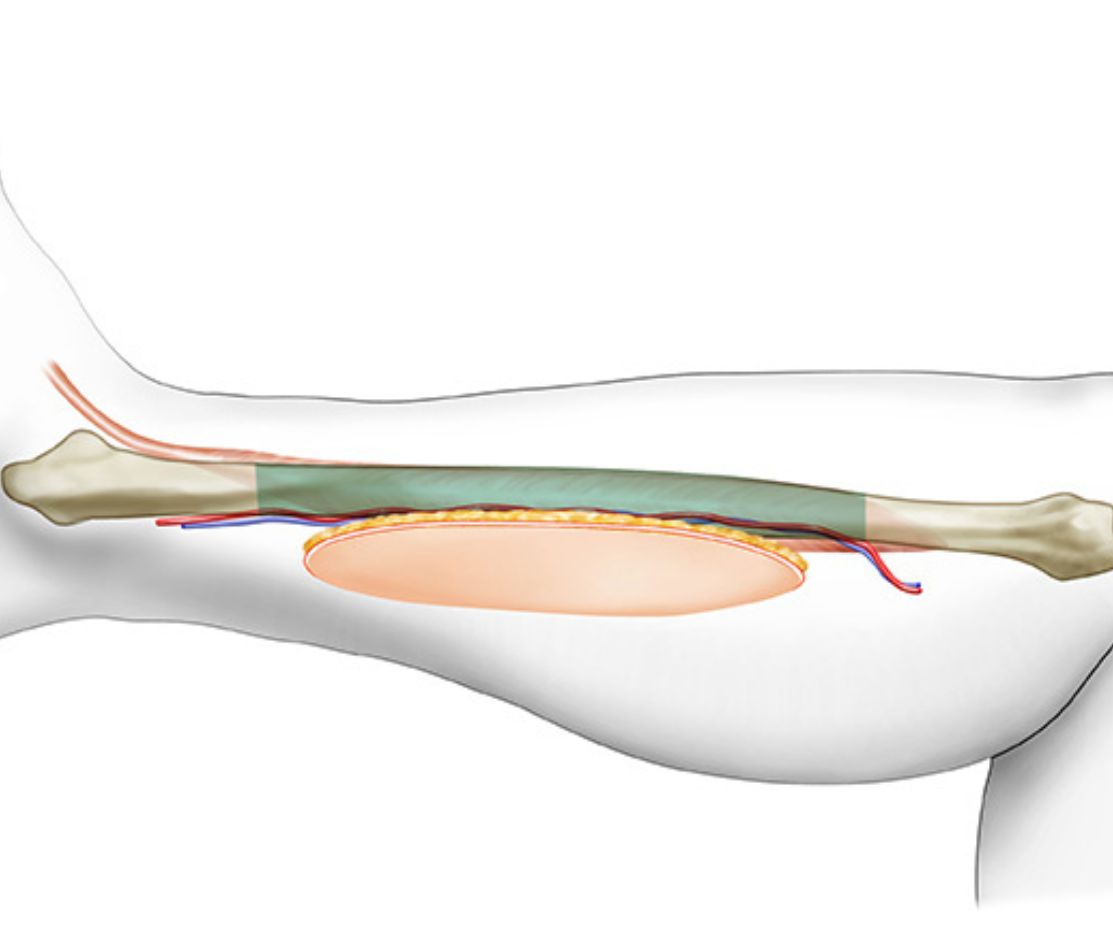
What Is a Free Fibula Osteocutaneous Flap?
- The fibula is the smaller bone in your lower leg (below the knee). You don’t need the entire bone to walk normally—so a portion of it can be used safely.
- “Osteo” means bone, and “cutaneous” means skin.
- This flap includes a segment of bone, along with skin and its blood vessels from the leg.
How Is the Surgery Done?
Removal of Affected Jawbone:
The damaged or cancer-affected part of the jaw is surgically removed.
Harvesting the Fibula Flap:
A piece of fibula bone, with its skin and blood vessels, is taken from the patient’s leg.
Shaping the Fibula:
The fibula bone is cut and shaped to match the jawbone that was removed.
Rebuilding the Jaw:
The shaped fibula is attached to the jaw area using titanium plates and screws.
Microsurgery:
The flap’s blood vessels are connected to neck vessels under a microscope, ensuring proper blood supply to keep the new jawbone alive.
Donor Skin Grafting:
The region of the leg where the skin has been taken is covered using small sheet of skin (skin graft) from the thigh.
*In selected cases teeth can also be placed over this jaw bone during the same surgery.
Why Use the Fibula?
- It’s strong and long enough to replace the jaw.
- It allows dental implants later on.
- The skin part helps rebuild the mucosa (inside of the mouth) if soft tissue is also missing.
- The leg usually heals well with minimal impact on walking.
What’s Recovery Like?
- Patients typically stay in the hospital for 4 to 6days.
- A feeding tube (Ryle’s tube) inserted via the nose may be used at first to maintain
nutrition. - Speech and swallow therapy helps recovery.
- The leg heals well; people walk normally after recovery
Benefits:
- Restores facial symmetry
- Improves ability to chew and speak
- Allows placement of teeth/dental implants later
- Boosts confidence and quality of life
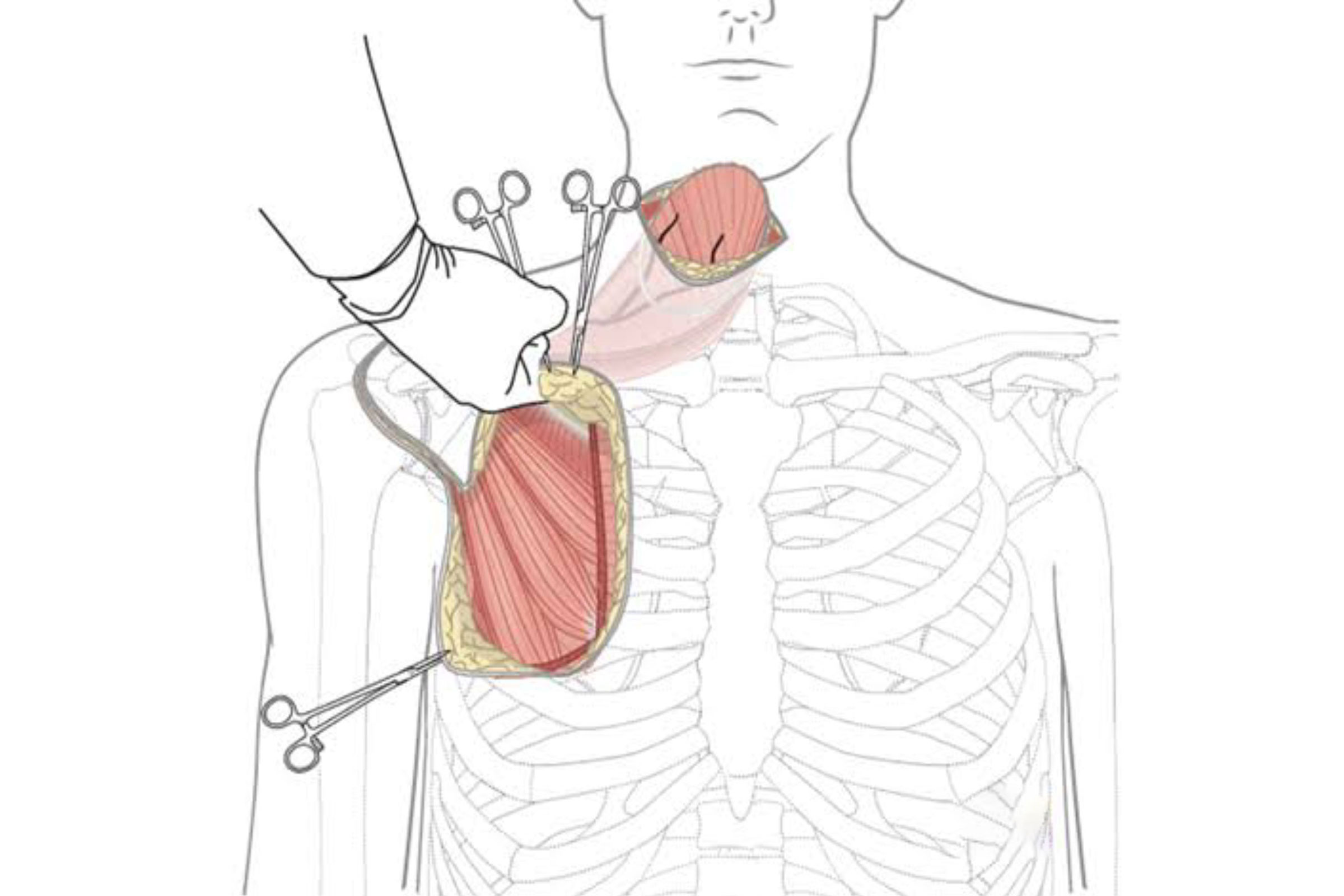
Free Scapular-Parascapular Flap:
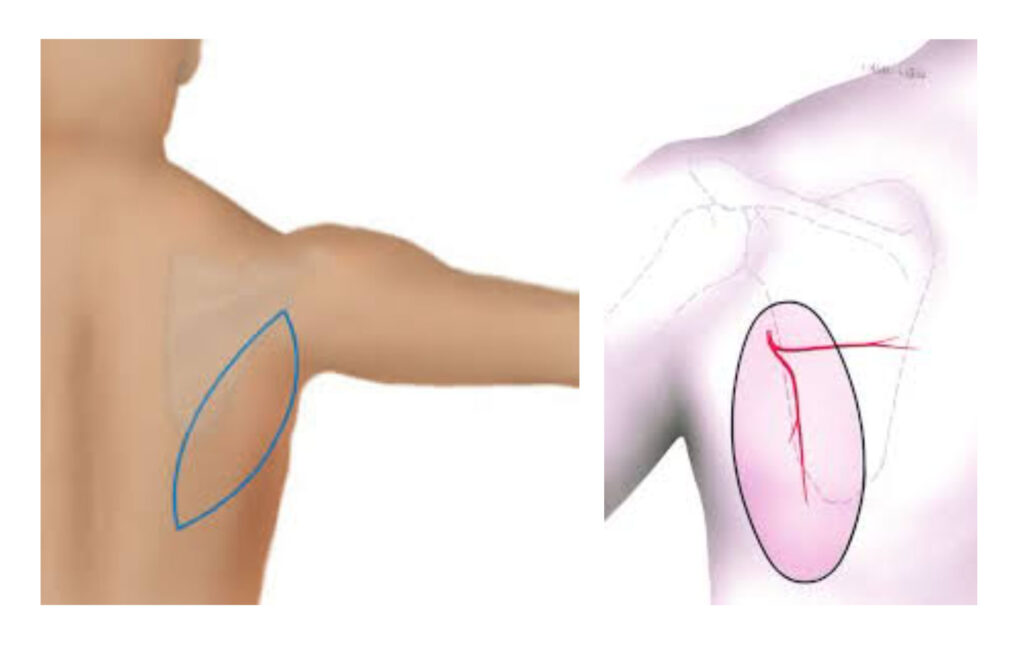
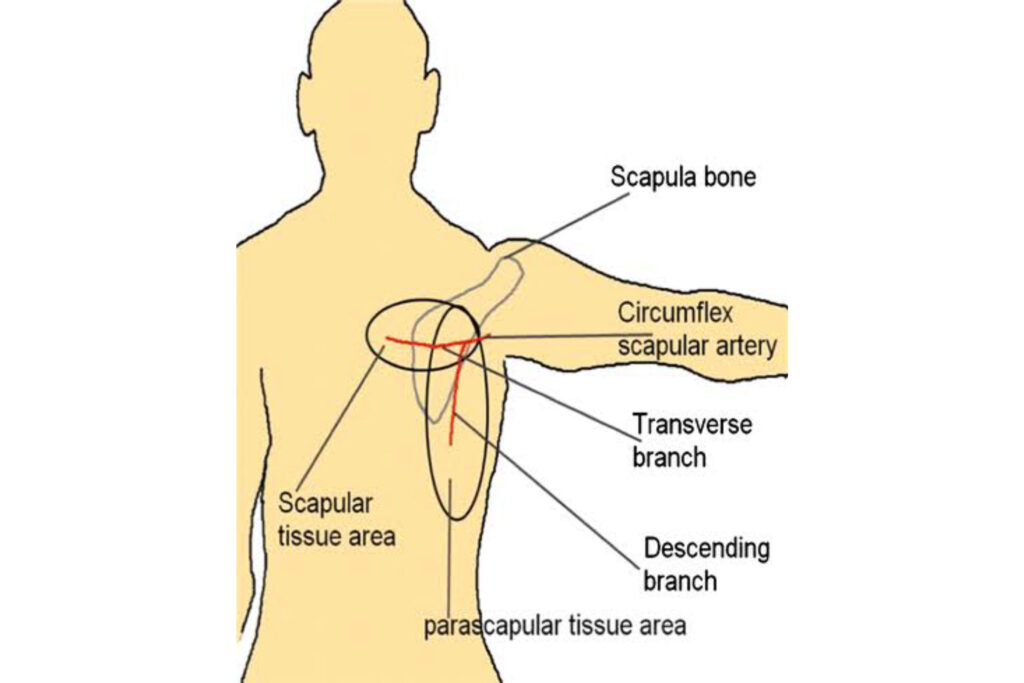
What is a Scapular-Parascapular Flap?
How Does the Surgery Work?
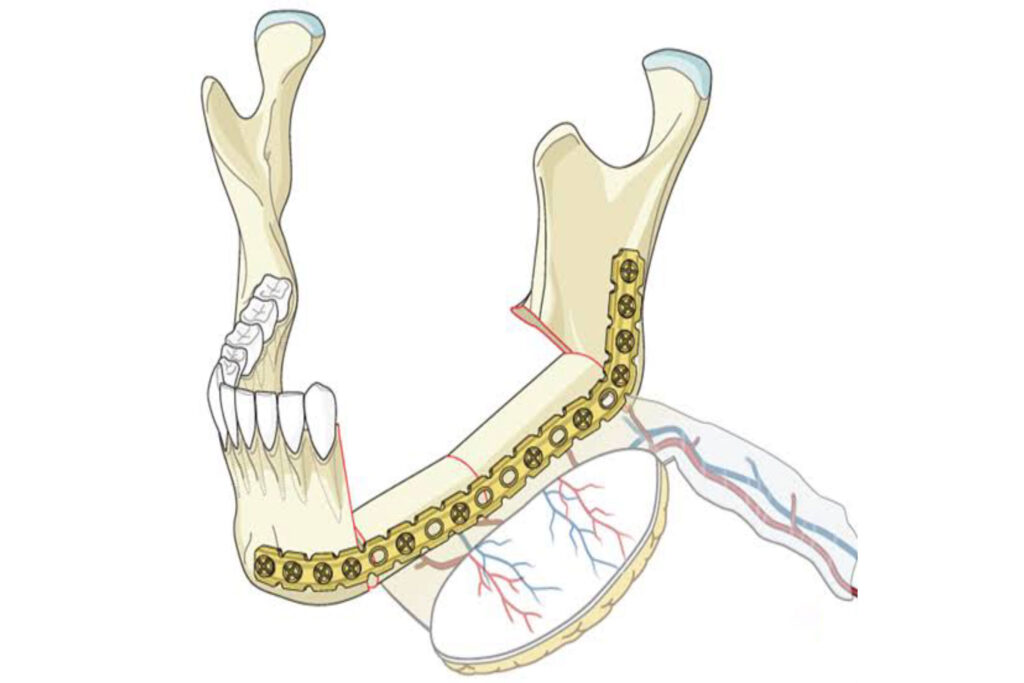
1. The cancerous/damaged jawbone is removed.
2. The surgeon then removes skin, tissue, and/or bone from the patient’s back (near the scapula).
3. These are shaped and placed in the jaw area to recreate the missing parts.
4. The tiny blood vessels from the flap are reconnected under a microscope to blood vessels in the neck to keep the flap alive.
Why Choose a Scapular Flap?
- It gives good-quality soft tissue to recreate the inside of the mouth or cheek.
- It can also provide bone, to rebuild parts of the jaw.
- The donor site (back) heals well and doesn’t affect shoulder movement much.
- It’s especially useful when a large amount of soft tissue is needed for reconstruction
What is Recovery Like?
- The patient may stay in the hospital for 5-6 days.
- A feeding tube (Ryle’s tube) inserted via the nose may be used at first to maintain
nutrition. - Speech and swallow therapy is started early.
- The back heals well, with a scar hidden near the shoulder blade.
- Over time, the person can chew, speak, and look more like themselves again
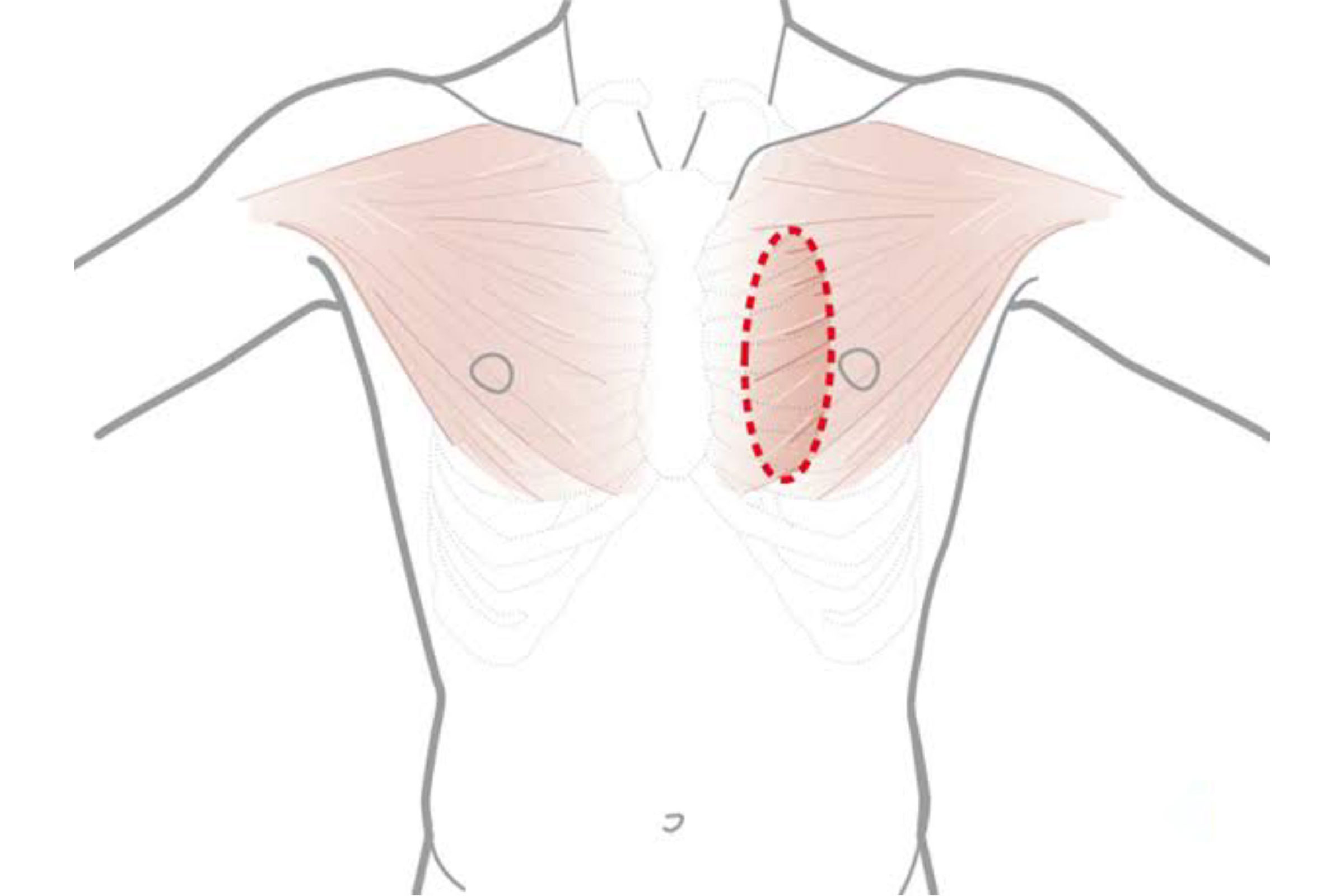
Pectoralis Major Myocutaenous flap (PMMC):
What Is a PMMC Flap?
- A pedicled flap using tissue from the pectoralis major (chest muscle), including skin, muscle, and blood vessels.
- It’s rotated up from the chest into the face and neck—no need for microsurgery (Joining blood vessels)
How the Surgery Works
1. The damaged part of the jaw is removed.
2. Surgeon shapes the PMMC flap on the chest—skin, muscle, and vessels together.
3. The flap is rotated to the head/neck through a tunnel under the skin.
4. The flap is stitched into place, addressing soft tissue defect.
BONE IS NOT RECONSTRUCTED IN THIS SURGERY
What to Expect in Recovery
- Hospital stay: 3-5 days.
- May need a feeding tube initially.
- Early physiotherapy helps with swallowing and speaking.
- Most patients regain decent function, complications occur but are usually manageable
Who Is a Good Candidate?
- Patients in resource-limited settings or with comorbidities.
- Useful when a free flap fails or isn’t feasible due to health/surgical constraints
But Here’s Why It’s Not Ideal for Rebuilding the Jaw:
“The PMMC flap is like a band-aid for the face. It can help cover a wound, but it doesn’t rebuild the jaw. It’s used only when better options like bone flaps from the leg (fibula) or back (scapula) aren’t possible.”
- The PMMC flap is made of soft tissue only—no bone.
- That means it cannot recreate the jawbone itself.
- So, it’s not a true reconstruction of the mandible—just soft tissue coverage
- “Think of it like covering a broken wall with a curtain, instead of rebuilding it with bricks.”
- The flap is often bulky and thick, which can leave the face unbalanced or unnatural
looking. - It doesn’t restore the original shape or contour of the jaw.
- Since there is no bone support, chewing, speech, and jaw movement may remain
impaired. - Dental implants or artificial teeth cannot be placed on a soft tissue flap.
- The chest flap may develop partial skin loss, wound infection, or fluid collection.
- There’s also a visible chest scar, and it may pull or stretch over time
- PMMC flaps were popular before microvascular free flap techniques were widely available.
- Today, they are considered a backup option in hospitals where modern reconstruction
(like fibula or scapula flaps) is not feasible.
Get In Touch
Schedule a consultation, ask questions, or explore our expert reconstructive surgery services and compassionate care.